Over the past 2 and a half years, the COVID-19 pandemic fundamentally shifted how we think about our health and the health of our population. With many Americans keeping a close eye on their finances, managing stress about global politics, working from home, and limiting their travel, an area of particular interest has been mental health.
Mental health conditions certainly existed prior to 2020, but the pandemic increased the need to address these common illnesses and the stigma around them. New research finds that mental health has replaced COVID-19 as the top health concern among Americans, but deeper analysis needs to be done into whether depression and anxiety are becoming more widespread, people are more willing to discuss these once-stigmatized conditions, or more researchers are studying mental health more broadly.
One way to measure the increase in prevalence and treatment of mental health issues is by looking at long-term prescribing data trends. Although large pharmacy benefit managers reported increased orders for medications that help patients manage depression and anxiety early in the pandemic, many assume these increases occurred because patients were hesitant to visit their physicians in person and were stockpiling medications, often increasing from 30-day supplies to 90-day supplies.
Some surveys have reported increased use of prescription medications to support mental health. However, these surveys asked whether individuals took any medication in the past 4 weeks to help manage emotions, concentration, behavior, or mental health, and are subject to measurement errors based on response rates and accuracy.
Aggregated, point-in-time data are often directionally helpful, but lack the specificity needed to understand deeper trends related to particular medication types or population-level behaviors. To dig deeper into mental and behavioral health trends, Arrive Health looked at transaction volumes occurring within a commonly used real-time prescription benefit (RTPB) tool.
Prescription Transaction Data
Arrive Health offers RTPB services to more than 2000 hospital and health system sites, with over 200,000 providers completing more than 7 million prescription transactions per month. A retrospective review of 12.44 million prescription transactions for mental and behavioral health medications was conducted between February 1, 2020, and July 31, 2022.
It is important to note that these services provide a connection between electronic health record (EHR) workflow and pharmacy benefit management companies. Therefore, the data in this report represent medications pended in the electronic prescribing workflow—when a physician inputs a medication into the ordering window in their EHR—not necessarily the final medication sent to the pharmacy or confirmation that the patient picked up the medication.
Because the size of the Arrive Health network changes as health systems, providers, and PBMs enable RTPB, the analysis and charts below represent the percentage of our total prescription transaction volumes, which include medications in the following classes:
- Antianxiety (benzodiazepines and more)
- Antidepressant (SSRIs, SNRIs, TCAs, and more)
- Antipsychotic (atypical and first-generation antipsychotics)
- Stimulant therapies for attention-deficit hyperactivity disorder (ADHD)
- Sedatives (hypnotics)
Key Findings and Transaction Trends
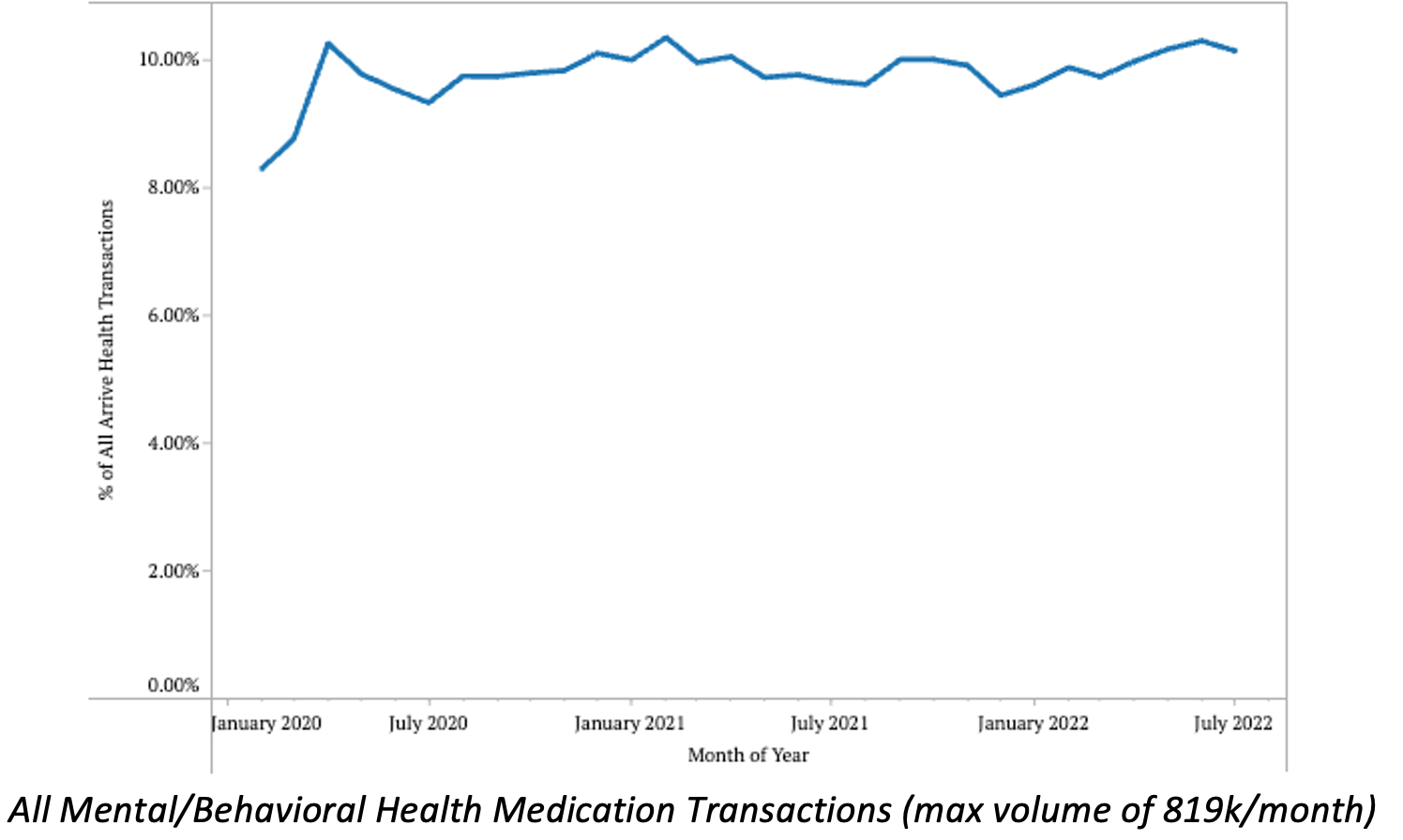
Data show that although prescription volumes for behavioral and mental health medications surged in early-2020 (likely due to the aforementioned reasons), volumes only slightly increased across 2020 and seemed to have leveled out or decreased slightly over the course of the next 2 years. At its highest, nearly 820,000 transactions for mental/behavioral health medications took place in May 2022, representing nearly 10% of the total prescription transaction volumes in the network and demonstrating the prevalence of the drug classes being looked at.
Arrive Health reported significant increases in certain medication transactions in early 2020, including chloroquine, hydroxychloroquine, and albuterol. Increases ranged from 50% to nearly 125% and were likely caused by surging publicity around these treatment options.
We followed-up our initial post with data showing significant decreases in orders for these medications. The changes in prescription volumes we’re seeing for mental/behavioral health medications are much smaller in comparison.
Below, we highlight some of the interesting trends we uncovered in our data:
- Between 2020 and mid-2022, pended medication volumes for mental/behavioral health medications remained within 9% and 10% of the total transaction volumes in our network.
- Since January 2022, we have seen a slight upward trend in mental/behavioral health transactions across our network.
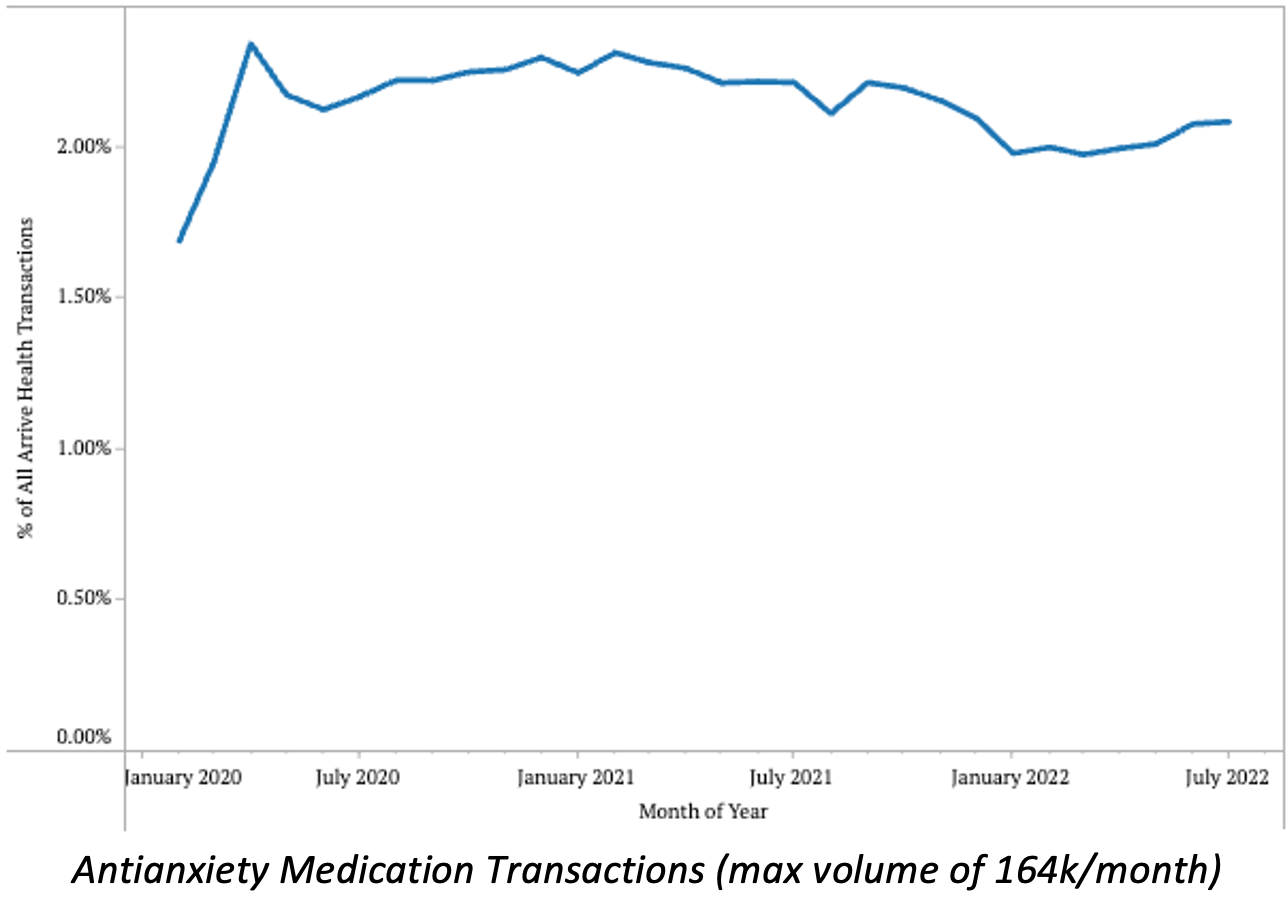
- Antianxiety medication transaction volumes have decreased steadily from their peak of 2.34% in early 2021, to 1.97% in early 2022, but are on a slight upward trend in 2022.
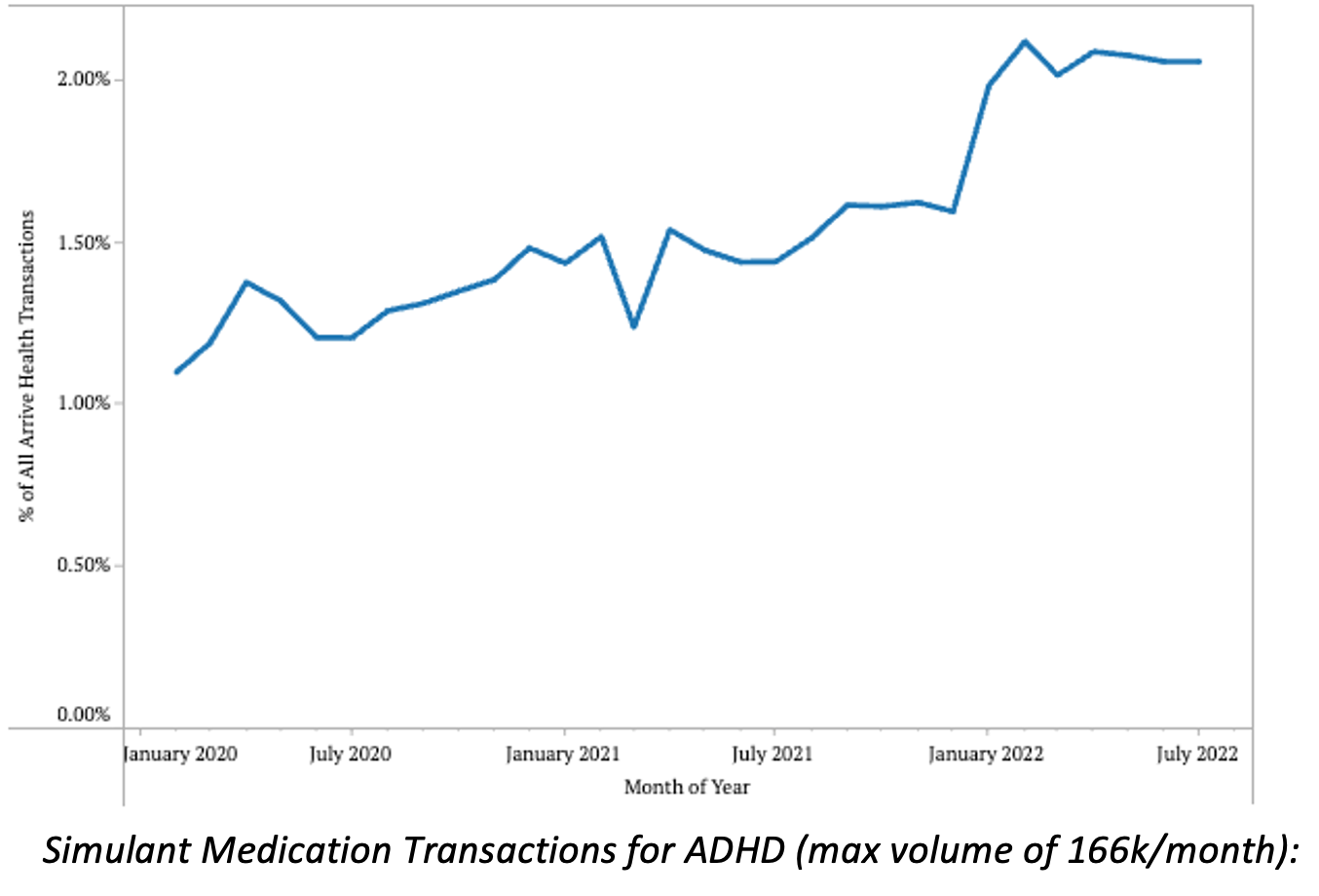
- Stimulant medications for ADHD saw transactions significantly increase over the past 2.5 years, from a low of 1.1% in February 2020 to 2.05% in July 2022
- Reports support these data, and state that ADHD rates are rising in adults and have been stable or increased in children.
- Some hypothesize that increases in ADHD diagnoses are connected to the influx of adults and students working/studying from home.
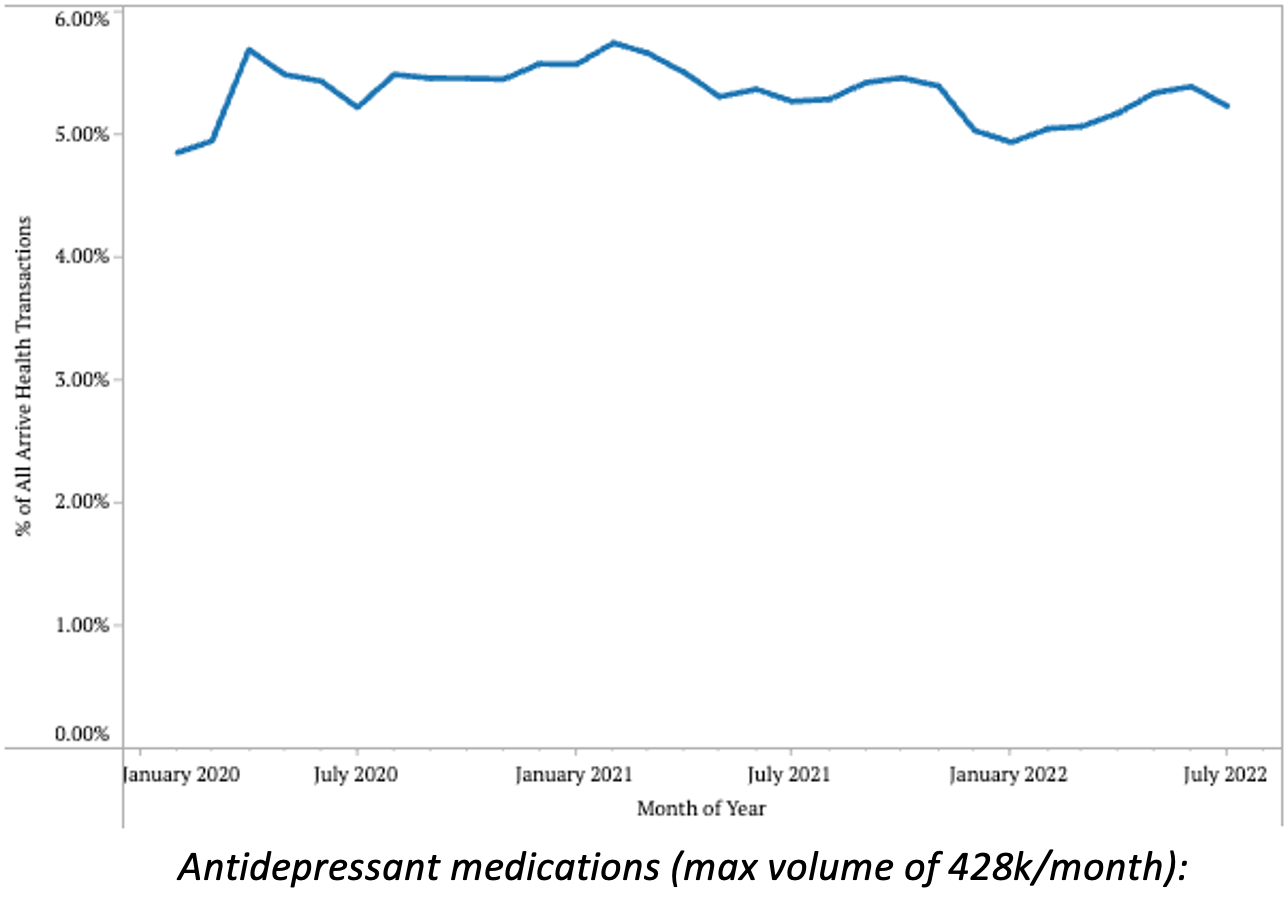
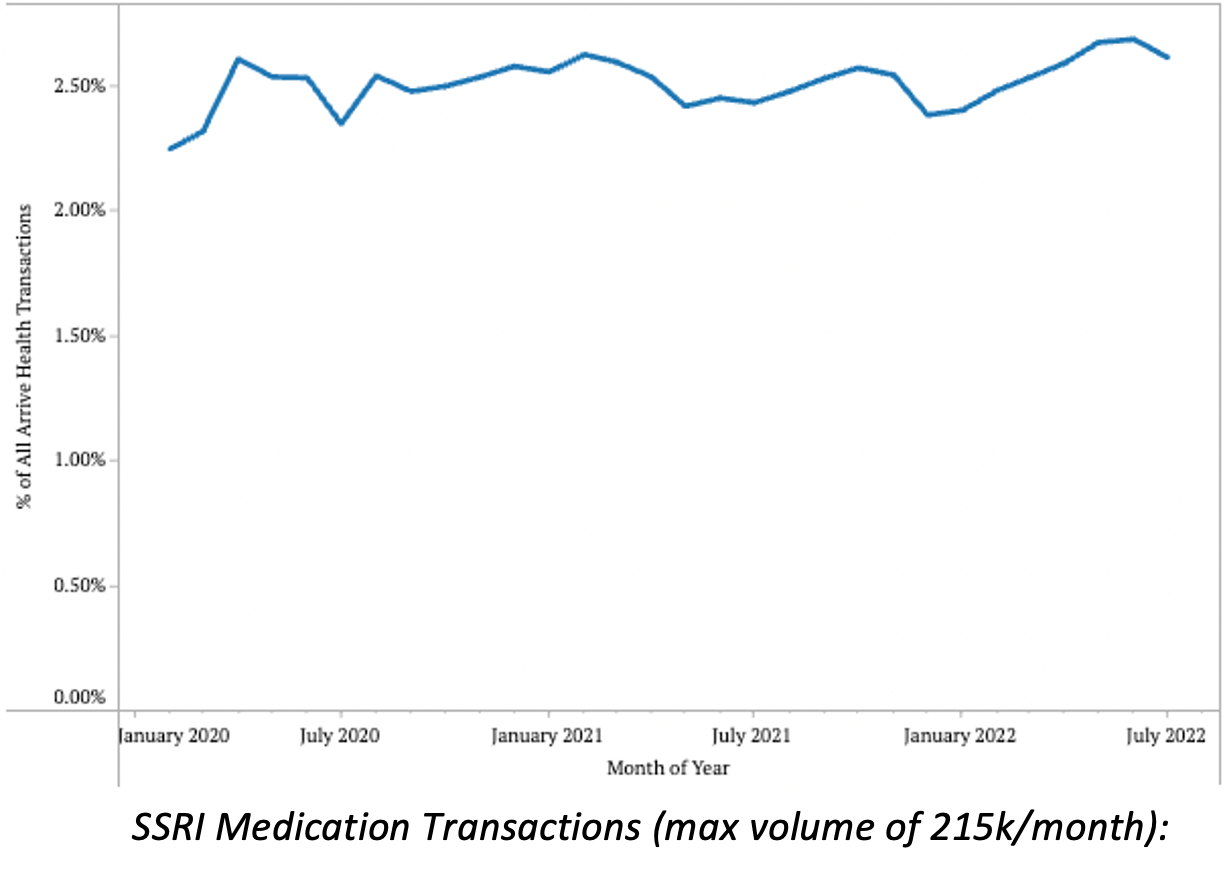
- Antidepressant therapy transactions saw slight increases in February 2021, October 2021, and June 2022. However, total volumes across the past 2.5 years have remained between 4.84% and 5.73%, indicating only slight changes in total prescribing volumes.
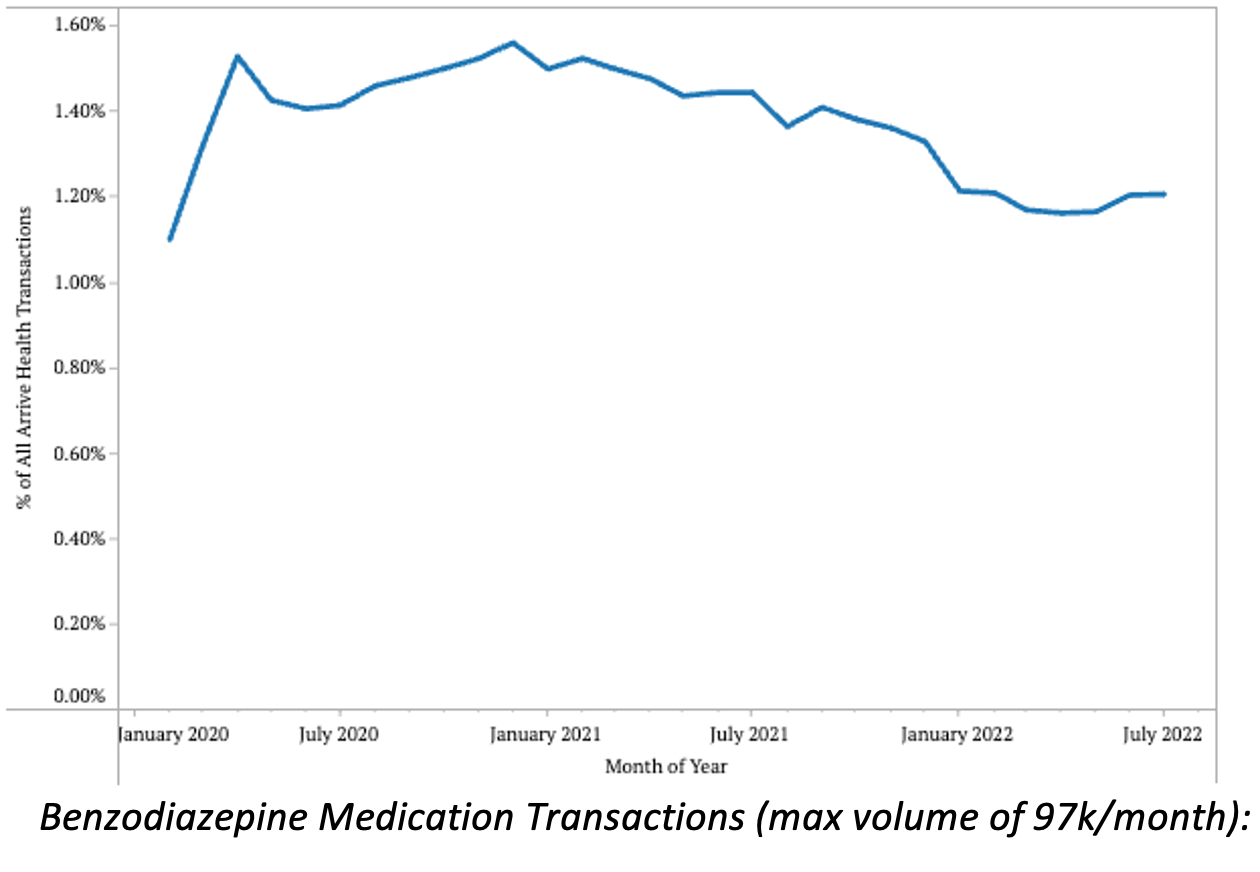
- JAMA recently looked at prescribing trends for benzodiazepines across the last 3 years and saw interesting results. In their report, they saw a slightly decreasing volume of benzodiazepine prescriptions (with a spike in early 2020), which matches the reduction in benzodiazepine transactions we saw over time.
- Steady decreases like this could be due to many factors, which should be studied more. Factors may include, but are not limited to, fewer patients diagnosed with anxiety or insomnia, providers finding the medication to be less effective, or stigma surrounding a medication making its use less common.
- One area to continue investigating is volumes of SSRI/SNRIs, which fluctuated more in our data compared to the JAMA research, which indicated small, but consistent, increases in prescription volumes month-over-month.
Driving Access to Essential Medication Classes
While the Arrive Health data represent more than 12 million prescription transactions, this information is not meant to be a scientific study or definitive representation of mental or behavioral health issues in America. Instead, we hope to shed light into the broader trends we are seeing in our data.
Unfortunately, there are still significant barriers for patients to receive these types of critical medications, including prior authorization and cost. Research shows that an increase of just $10 can reduce medication adherence by upwards of 10%-20%. Further, the AMA found that prior authorization processes are reported to cause care delays 93% of the time.
Looking at the same 12.44 million transactions previously measured, we calculated that 34% of the time, there was an opportunity for the provider to select a lower-cost medication option (totaling $114 million in potential patient savings). Further, 366,000 patients were seen in which there was an opportunity to avoid a coverage restriction, including age restriction, out-of-network pharmacy, not on formulary, quantity limit, and drug form.
Where We Go From Here
It is essential that we continue to study mental health and its treatments. The industry must also do more to examine specific barriers to mental health care and understand trends in medication availability, cost, and use.
For example, is the volume reduction in benzodiazepine transactions due to anxiety becoming less common? Or are physicians less confident in the medication’s efficacy? Or are there cost barriers that are preventing refills or driving abandonment?
Fortunately, there are ongoing efforts to destigmatize mental and behavioral health and normalize its treatment nationwide. In particular, the government has put an emphasis on making mental health resources more widely available and requiring coverage for many mental health treatments.
Through a combination of policy changes and technological innovation, the industry can improve access to essential medications by breaking down barriers to care and reducing costs for patients.

